Key Takeaways
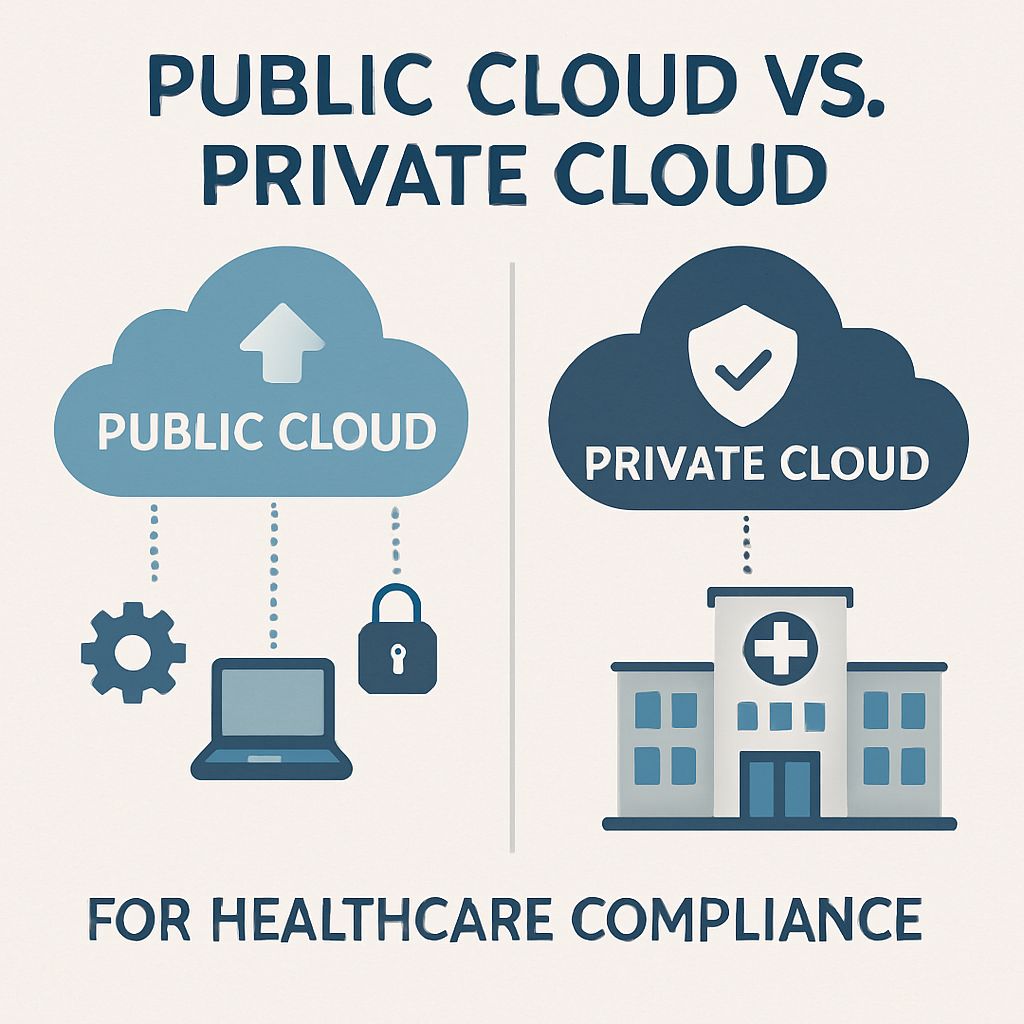
- When it comes to choosing between public, private, or hybrid cloud solutions for PHI data, healthcare organizations need to make HIPAA compliance a top priority.
- Public cloud providers like AWS, Azure, and GCP offer services that are HIPAA-eligible, but healthcare organizations need to understand their responsibilities under the shared security model.
- Private cloud environments offer the most control over PHI data but come with higher costs and infrastructure management responsibilities.
- For many healthcare organizations, a hybrid cloud approach offers the best balance between security, compliance, and operational efficiency.
- Working with cloud providers that have experience with healthcare compliance requirements can significantly reduce migration risks and ensure that you stay in line with regulations over the long term.
Migrating to the cloud in healthcare isn’t just a decision for IT—it’s a critical compliance decision that affects the security of patient data, operational efficiency, and the legal standing of your organization. Making the wrong move can result in expensive HIPAA violations, while the right strategy can lead to innovation without sacrificing security.
When it comes to healthcare cloud migration, it’s critical to consider compliance requirements, particularly when handling protected health information (PHI). At SlickFinch, we’ve successfully led many healthcare organizations through secure cloud transitions, aiding them in navigating the complex regulatory landscape while reaping the benefits of cloud computing.
Knowing what you’re dealing with—whether it’s public, private, or hybrid cloud infrastructures—is crucial for making choices that both keep patient data safe and allow for digital transformation. Let’s look at the key things to think about for each method.
Healthcare Cloud Compliance: A High-Stakes Game
Healthcare organizations face a set of unique regulatory requirements that heavily influence their decisions about migrating to the cloud. Compliance with HIPAA isn’t a choice—it’s a legal obligation, and the penalties for not complying can be severe. The Office for Civil Rights has handed out fines of over $1.8 million for failures to comply with cloud-related regulations, highlighting the seriousness of mistakes in this area.
In addition to HIPAA, healthcare cloud environments may need to meet other standards such as HITRUST CSF, SOC 2 Type II, and FedRAMP certifications, depending on your specific operations. Each cloud model – public, private or hybrid – presents unique compliance advantages and challenges that must be balanced against your organization’s specific needs, technical requirements, and risk tolerance.
Grasping the subtleties of these compliance frameworks is not just about dodging penalties—it’s about building a base of trust with patients who expect their sensitive information to be private and secure. This duty goes beyond ticking regulatory boxes to truly effective security practices.
The Pros and Cons of Public Cloud in Healthcare
Public cloud platforms have come a long way in terms of their healthcare compliance capabilities, with advanced tools that can actually boost security when set up correctly. The cost efficiencies provided by big players such as AWS, Azure, and Google Cloud, thanks to their economies of scale, are attractive to many healthcare organizations, particularly those dealing with variable workloads or fast expansion.
Benefits of Cost Efficiency and Scalability
Public cloud services work on a pay-as-you-go model which saves healthcare organizations from having to make significant initial investments in infrastructure. This operational expense model allows healthcare organizations to align their costs with their actual usage patterns. This could potentially reduce their total IT spend while also improving their financial predictability. Traditional on-premises solutions cannot match the operational agility provided by the ability to rapidly scale resources up or down during periods of patient surge or when launching new digital health initiatives. For a detailed comparison, you can explore the best HIPAA compliance options across different cloud providers.
Several healthcare institutions have discovered that public cloud platforms allow for quicker rollouts of new applications and services, reducing the time it takes for digital health advancements to create value. In competitive healthcare markets, this ability to implement changes quickly can be especially beneficial, as being the first to introduce new patient services can give an organization a strategic edge.
Services from Major Providers that are HIPAA-Compliant
Major cloud providers such as AWS, Azure, and Google Cloud have all created a wide range of HIPAA-eligible services that are specifically tailored for healthcare workloads. They are willing to sign Business Associate Agreements (BAAs), which legally obligate them to put in place the necessary safeguards for PHI. Their compliance certifications often go above and beyond what HIPAA requires, offering extra layers of security through frameworks such as HITRUST CSF.
These platforms come with advanced encryption features for data at rest and in transit, detailed access controls, and comprehensive audit logging—all of which are crucial for HIPAA compliance. Several also offer healthcare-specific services such as medical imaging storage, healthcare API integration tools, and machine learning features tailored for clinical applications.
Major Cloud Provider HIPAA Capabilities Comparison
AWS: HIPAA-eligible services, BAA available, HITRUST CSF, dedicated healthcare team
Azure: HIPAA compliance toolkit, BAA available, Azure Healthcare APIs, medical imaging service
Google Cloud: HIPAA compliance, BAA available, Healthcare Natural Language API, healthcare data engine
Shared Responsibility Model: What Falls on You
A critical concept often misunderstood in healthcare cloud deployments is the shared responsibility model. While cloud providers secure the infrastructure itself, healthcare organizations remain responsible for properly configuring cloud services, managing access controls, and ensuring application-level security. This division of responsibilities creates potential compliance gaps when not clearly understood and addressed.
Many HIPAA violations in cloud environments stem from misconfigurations rather than provider failures. For example, improperly configured storage buckets have led to multiple high-profile PHI exposures. Healthcare organizations must implement rigorous change management processes, security testing, and compliance validation for every cloud deployment.
Healthcare organizations are typically responsible for encrypting PHI, implementing access controls, and maintaining audit logs, not the cloud provider. This requires specialized expertise that many healthcare IT teams may not have, potentially requiring partnerships with security consultants who are experienced in healthcare cloud implementations.
Security Concerns in Shared Cloud Environments
Public cloud environments are shared spaces. This means that your healthcare data is stored on the same infrastructure as other organizations. Even though providers use advanced isolation mechanisms, some healthcare compliance officers worry about the possibility of vulnerabilities between tenants. These concerns need to be weighed against the strong security measures that major providers can implement on a large scale. For a detailed comparison of cloud providers, you can refer to this HIPAA compliance comparison of AWS, Azure, and GCP.
Major public clouds are attractive targets for sophisticated threat actors because they store valuable healthcare data. However, leading cloud providers usually invest billions in security infrastructure that is more than what individual healthcare organizations could implement on their own. This creates a complex risk calculation that must consider both increased targeting and enhanced defensive capabilities.
Private Cloud Solutions: Total Control for PHI
Private cloud environments offer dedicated infrastructure either on-site or in specialized healthcare-focused hosting facilities. This strategy gives healthcare organizations total control over their compliance environment, eliminating the multi-tenant worries that come with public cloud deployments. For organizations with highly specialized compliance requirements or unique security needs, this control can be priceless.
When Total Control Over Data Is Crucial
There are healthcare organizations that handle highly sensitive data or operate under very strict regulations. These organizations need to know exactly where their data is located, who has access to it, and how it is being processed. Private clouds give them total control over their data, allowing them to decide exactly where their PHI is located and who has access to it and under what conditions.
Private settings also offer the opportunity to incorporate security controls specific to healthcare that may not be available or adjustable in standardized public cloud offerings. This customization can be especially beneficial for specialized clinical workflows with unique security needs or legacy systems with specific compatibility requirements.
Dealing with Outdated Systems
Many healthcare organizations still use old, mission-critical systems that were not built to be used in the cloud. These systems often use old protocols, need certain network settings, or have dependencies that make it difficult to move to a public cloud. However, private clouds can be customized to work with these outdated systems while still offering some benefits of the cloud. For more insights, check out this legacy application migration checklist.
Private clouds are ideal for intricate healthcare integration situations because they allow for personalized networking, storage configurations, and security controls. If clinical workflows require close integration between systems, the controlled environment of a private cloud usually offers more consistent performance and easier troubleshooting.
What You’ll Really Pay for Private Cloud Compliance
Even though private clouds come with some compliance benefits, they also come with a much heftier price tag and more operational duties. Companies have to pay for the whole infrastructure rather than splitting the cost with other users like they would in a public cloud. This usually means higher costs per workload and the need to keep extra capacity to handle peak demands.
Private cloud deployments also significantly increase staffing requirements. Healthcare organizations need to keep up with infrastructure management, security operations, and compliance monitoring—skills that are becoming harder and costlier to recruit and retain. When total ownership costs are calculated, these hidden costs often make private clouds more expensive than expected.
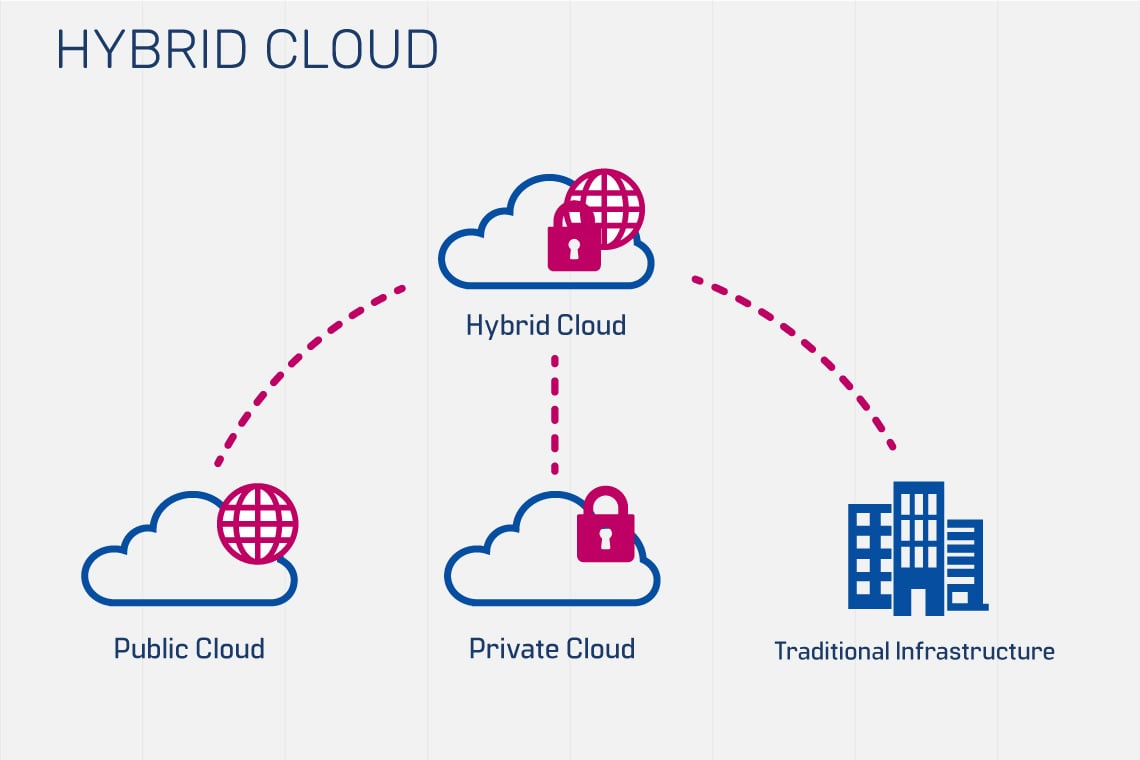
Hybrid Models: A Perfect Blend?
Several healthcare organizations are discovering that hybrid cloud methods provide an ideal equilibrium between compliance management and operational productivity. This model enables the placement of the most sensitive PHI workloads in private settings while utilizing public clouds for less sensitive applications, analytics, and client-facing services.
“Healthcare Cloud Computing – A …” from techvify.com and used with no modifications.
Strategic Frameworks for Data Separation
Effective hybrid strategies start with a comprehensive framework for data classification. This identifies different types of information based on sensitivity, compliance requirements, and operational needs. This classification guides decisions about where specific data and workloads should reside. This allows for risk-appropriate placement decisions rather than one-size-fits-all approaches.
For instance, research datasets that have been de-identified might be situated in public cloud environments in order to take advantage of superior analytics capabilities, while the information that could be used to identify someone remains in private environments that are more controlled. Similarly, patient portals might operate in scalable public clouds while the clinical systems they connect to remain in private infrastructure.
- Highly sensitive: Direct patient identifiers, detailed clinical records, payment information
- Moderately sensitive: Partially de-identified clinical data, operational records, scheduling systems
- Less sensitive: Fully de-identified research data, public-facing content, non-clinical applications
- Not sensitive: Marketing content, publicly available information, general business applications
This graduated approach allows organizations to match security controls and environments with actual risk levels instead of treating all systems as equally sensitive. The result is more cost-effective compliance without sacrificing security where it matters most.
Creating Compliant Data Transfers Between Environments
Hybrid structures necessitate the safe, compliant transfer of data between environments. This integration layer necessitates meticulous design to ensure compliance from start to finish across the hybrid environment. To ensure that PHI remains safe as it travels through various cloud environments, encrypted APIs, secure gateways, and complete audit trails must be established.
Healthcare institutions frequently use API gateways that have security features tailored to the healthcare sector to handle these intricate data flows. These gateways can ensure consistent authentication, authorization, and encryption policies, no matter where the data comes from or how it’s processed. Additionally, they offer the extensive logging necessary for demonstrating compliance during audits.
In the world of hybrid healthcare, syncing data between environments can be tricky. To keep everything consistent across platforms while still keeping sensitive information separate, organizations need to have strong reconciliation processes in place. This usually means developing custom integrations that take into account the specific compliance issues that come with healthcare.
Choosing Where to Place Workloads
Deciding where specific healthcare workloads should go requires a structured evaluation framework. The framework should take into account technical requirements, compliance considerations, performance needs, and cost factors. Many organizations develop formal decision matrices to guide them in deciding where to place workloads. This is a more reliable method than going by gut instinct.
Workloads that are operational and have predictable resource needs are often more cost-effective in private environments, while those that are variable can take advantage of the elasticity of the public cloud. Similarly, development and test environments can often be cost-effectively run on public clouds, while production environments that handle protected health information (PHI) may need to be run on private infrastructure. Making these nuanced decisions requires both technical and compliance expertise.
Non-negotiable Technical Safeguards for Any Cloud Environment
No matter the cloud model you choose, there are technical safeguards that are a must for healthcare deployments. These controls are the building blocks of HIPAA compliance and need to be consistently implemented across all environments that house or process PHI.
Keeping PHI Safe: Encryption for Data at Rest and in Transit
Healthcare organizations have to comply with HIPAA regulations, which include encryption for PHI both when it is being stored (at rest) and when it is being transmitted (in transit). In the cloud, this usually involves using AES-256 encryption for storage and TLS 1.2 or higher for all network communications. Some healthcare organizations also use field-level encryption for especially sensitive data elements, providing extra protection beyond standard database encryption.
Managing keys is especially important in cloud environments. Healthcare organizations must keep control of encryption keys while implementing rotation policies and secure backup procedures. Hardware Security Modules (HSMs) often play a role in these architectures, providing FIPS-validated key protection even in public cloud environments.
Managing Access and Identities
For healthcare compliance in the cloud, it’s important to implement the principle of least privilege through role-based access controls. This means that each user should only have the access they need for their job function and nothing more. This level of detailed permission management needs to be applied across all cloud environments, which will require advanced identity federation and access management solutions.
Healthcare cloud environments now consider multi-factor authentication as a standard requirement, serving as a crucial layer of protection against the compromise of credentials. Identity validation is strengthened by biometric authentication, hardware tokens, and mobile verification apps, which are more effective than passwords alone. These controls should be consistently implemented across all entry points to cloud resources that contain PHI.
Tracking Systems and Oversight
Complete audit trails that record who accessed which data, when they accessed it, and where they accessed it from are critical for both security and compliance. Cloud environments need to be set up to record detailed access logs for all PHI interactions. These logs should be kept in systems that are resistant to tampering and should be kept for as long as regulations require, which is often longer than the standard retention period.
Systems that monitor automatically must be constantly scrutinizing these logs for any patterns that might seem suspicious and could indicate a security incident. Anomaly detection that is based on machine learning has become increasingly valuable for identifying attacks that are subtle and might otherwise go unnoticed in complex healthcare environments. These systems that monitor should generate alerts that are actionable and have enough context for a rapid investigation.
Planning for Disaster Recovery and Business Continuity
Healthcare organizations have to ensure that they have non-stop access to their critical clinical systems. This makes it very important to have solid disaster recovery capabilities in any cloud strategy. The Recovery Point Objectives (RPO) and Recovery Time Objectives (RTO) must be officially established for each system. This should be based on how important the system is to patient care and operations. Cloud architectures should be set up to meet or exceed these objectives. This can be done through suitable redundancy and failover mechanisms.
It is both a requirement for compliance and a practical necessity to regularly test recovery procedures. These tests should mimic a variety of failure scenarios to ensure that systems can be restored within the necessary timeframes. Documentation of these tests is a critical component of demonstrating due diligence during compliance audits.
Protocols for Security Incident Responses
Cloud settings necessitate unique incident response protocols that recognize the shared responsibility model and restricted access to infrastructure. Healthcare institutions need to establish playbooks specifically for the cloud for identifying, controlling, and rectifying security incidents. These protocols should clearly delineate the roles and responsibilities of the organization and cloud providers.
Healthcare incident response is particularly urgent due to HIPAA’s breach notification requirements. Organizations need to be ready to determine quickly if an incident is a reportable breach. This means they need forensic capabilities that work well in cloud environments. If organizations have pre-established relationships with cloud provider security teams, they can respond to incidents much more effectively.
Legal Considerations: BAAs and More
Business Associate Agreements are the cornerstone of healthcare cloud deployment legality, but they’re only the tip of the iceberg when it comes to necessary contracts. These agreements need to clearly outline breach notification schedules, security incident responsibilities, and how liability is divided between parties.
Key Components of a BAA with a Cloud Provider
A well-structured BAA should clearly define the security responsibilities of your organization and the cloud provider. The BAA should lay out the timeframes for incident notification that allow you to comply with your HIPAA requirements, which typically require providers to notify you within 24-48 hours of identifying a potential breach that affects your data. The agreement should also cover data handling at the end of the relationship, ensuring proper procedures for returning or destroying data.
In addition to these fundamentals, healthcare institutions must advocate for the contractual right to audit or gain access to compliance reports that show continued compliance with security protocols. Security-related issues should be included in Service Level Agreements (SLAs), with financial penalties for non-compliance. These contractual safeguards offer a remedy if providers do not uphold the security measures they have promised.
How Liability is Shared in Various Cloud Models
When it comes to cloud models, there are differences in how liability is distributed. In the case of private clouds, organizations hold the majority of the responsibility, though some may be shared with managed service providers. Public clouds, on the other hand, operate under a more complex shared responsibility model. Here, providers are in charge of infrastructure security, while customers must take care of proper configuration, access control, and data protection.
Hybrid environments often present intricate liability situations that need to be thoroughly outlined in contracts. It’s crucial to have comprehensive documentation of security responsibility boundaries to avoid crucial controls from being overlooked between multiple providers and your internal teams. These responsibilities should be aligned with particular compliance requirements to guarantee comprehensive coverage.
Considerations for International Data Transfers
Healthcare organizations that operate on an international level must also consider data sovereignty. This adds a new level of complexity to their operations. Regulations such as the GDPR in Europe, or CCPA in the state of California, have strict requirements for cross-border data transfers. These requirements must be addressed in cloud architectures. It is important for healthcare organizations to know where their data physically resides. They must also understand how it moves between jurisdictions.
Cloud services provide region-specific deployments that can help keep data within the necessary geographic boundaries. But, organizations need to ensure that backup, disaster recovery, and support functions don’t accidentally move data across borders in a way that violates regulatory requirements. These considerations should be clearly addressed in cloud contracts and technical designs.
Assessment Phase: What Goes Where?
Before you move any healthcare workloads to the cloud, you should thoroughly evaluate your application portfolio. This evaluation should categorize systems based on how they handle PHI, technical requirements, integration dependencies, and the impact on compliance. The assessment forms a basis for making the right placement decisions instead of moving systems without a clear plan.
Start by documenting the current security controls, compliance requirements, and operational dependencies for each system. This will create a baseline that will help you identify any compliance gaps that need to be addressed in the target cloud environment before the migration can proceed safely. Many healthcare organizations find undocumented data flows during this process that have a significant impact on cloud architecture decisions.
Involve the clinical stakeholders in the early stages of the assessment process to understand the impact on workflows and the crucial system interdependencies that may not be evident to IT teams. Their insights can avoid disruptive migrations that are technically successful but cause operational issues for healthcare delivery.
Begin with Non-PHI Workloads
When you begin your cloud migration, start with non-PHI systems. These have less compliance risk. You can learn about cloud operations, security configurations, and performance management with these systems before you move on to more sensitive workloads. You might start with public-facing websites, learning management systems, or operational applications that don’t handle patient data.
Take advantage of these initial migrations to confirm your governance processes, security monitoring abilities, and operational procedures in the cloud setting. Make a record of the lessons you’ve learned and fine-tune your strategy based on these experiences. This step-by-step approach develops institutional cloud proficiency that greatly minimizes risk when migrating PHI workloads later.
Employee Education on Updated Compliance Rules
Cloud systems need different security methods than regular data centers, which means extensive employee education is required. Security teams have to comprehend the shared responsibility model and threats specific to the cloud. Development teams need to be educated on secure cloud setup and deployment methods that keep compliance through automation instead of manual processes. Depending on which cloud provider you choose, how security and compliance is handled varies greatly, and as a result so do the responsibilities on your teams. You can read more about how the main 3 providers vary and how that affects your teams and the overall business in this article.
Design training programs that cater to the unique compliance duties of various team members. Technical personnel require a comprehensive understanding of cloud security configurations, while compliance officers should be able to decipher cloud security documentation and audit evidence. Executive leadership needs to be educated on new risk profiles and governance considerations in cloud settings.
Implementation Timeline in Phases
It’s important to create a timeline that takes into account the complexities of healthcare cloud migrations. Most healthcare cloud transitions that are successful take anywhere from 18-36 months to fully complete, with critical PHI workloads typically moving later in the process once cloud operations have become more established. This phased approach allows for proper risk management while still making significant progress.
Be sure to include checkpoints for compliance validation in your migration timeline. These official assessments should confirm that security controls are functioning properly before increasing PHI processing in cloud environments. They should consist of both technical testing and document review to guarantee that both operational and administrative compliance requirements are met.
It’s important not to overlook the amount of time needed for contract negotiations, particularly for BAAs with cloud providers. These agreements often necessitate several rounds of review by legal, compliance, and technical teams to ensure all requirements are met. Starting these discussions early can help avoid delays when you’re technically ready to migrate.
- Phase 1: Assessment and planning (3-6 months)
- Phase 2: Non-PHI workload migration and operational validation (3-6 months)
- Phase 3: Limited PHI workload migration with enhanced monitoring (6-12 months)
- Phase 4: Enterprise-wide migration and optimization (6-12 months)
- Phase 5: Continuous compliance monitoring and improvement (ongoing)
How SlickFinch’s Expertise Can Help You Choose The Right Strategy
Navigating healthcare cloud migrations requires specialized expertise in both healthcare compliance and cloud technologies—a combination that’s increasingly rare in today’s market. SlickFinch’s healthcare cloud consultants bring huge experience from hundreds of successful healthcare migrations across all major cloud platforms. Our team includes HIPAA compliance specialists, cloud security architects, and healthcare IT veterans who understand both the technical and regulatory landscape.
Our team has created a unique Healthcare Cloud Readiness Assessment that pinpoints compliance discrepancies, technical needs, and organizational readiness elements that are unique to your situation. This assessment gives a straightforward plan for adopting the cloud that reduces risk while maximizing the benefits of cloud transformation for your healthcare organization.
The Compliance Framework of the Future
As healthcare compliance requirements continue to change, it is necessary to have cloud architectures that can adapt to the new regulations without requiring a complete overhaul. By building flexibility into your cloud strategy, you can respond to new requirements such as information blocking rules, increased patient access rights, and increased security requirements without disrupting operations.
|
Compliance Dimension |
Current Focus |
Emerging Requirements |
Cloud Strategy Implications |
|---|---|---|---|
|
Data Access |
Provider-controlled access |
Patient-directed sharing |
API-enabled architectures required |
|
Security Controls |
Perimeter-focused |
Identity-centered security models | |
|
Audit Requirements |
Access logging |
Behavioral analytics |
Advanced monitoring solutions needed |
|
Privacy Regulations |
HIPAA-focused |
State-specific requirements |
Configurable privacy controls by jurisdiction |
Healthcare organizations that succeed are putting in place cloud governance frameworks that anticipate these evolving requirements rather than just meeting current mandates. These forward-thinking approaches incorporate emerging standards like NIST’s zero-trust architecture guidelines and HL7’s FHIR standards for interoperability, positioning organizations to meet compliance requirements more efficiently as they emerge.
The best compliance frameworks are the ones that are integrated directly into cloud deployment pipelines, providing automated security validation and documentation generation. This approach, often referred to as “compliance-as-code,” guarantees that security requirements are consistently implemented across environments, and it also reduces the manual effort needed for audits and assessments.
Common Questions
Healthcare organizations often ask the same questions when considering their cloud migration options. These questions usually focus on regulatory compliance, security responsibilities, and operational considerations that are unique to healthcare environments. By answering these questions in advance, organizations can set realistic expectations and develop appropriate risk management strategies.
The responses given below are based on the latest industry standards. However, they should be assessed based on your organization’s specific needs, risk tolerance, and compliance requirements. It’s advisable to consult with qualified legal and technical advisors before making significant decisions about healthcare cloud migration.
Is it possible for public clouds to be as secure as private clouds when it comes to healthcare data?
Yes, public cloud environments that are properly set up can match or even surpass the security capabilities of most private clouds. Big providers such as AWS, Azure, and Google Cloud spend billions on security research, monitoring, and infrastructure protection, which few private environments can compete with. The main difference isn’t whether it’s public or private, but the quality of the implementation, security expertise, and governance controls that are applied. Organizations with strong cloud security skills and solid compliance processes can achieve HIPAA compliance in any cloud model. The biggest risks usually come from misconfiguration or insufficient security governance rather than limitations of the platform itself.
What if my cloud provider has a breach that exposes PHI?
In the event your cloud provider has a security breach that impacts your PHI, they must notify you within the timeframe agreed upon in your contract. This is required under your BAA. You are still responsible for determining whether the incident is a reportable breach under HIPAA. You are also responsible for notifying the affected individuals and regulatory authorities. This shows why it’s important to have clear incident response procedures that are integrated with your cloud provider’s processes. It also shows why it’s important to have contract terms that ensure you receive information about potential incidents in a timely manner. Many organizations set up escrow arrangements for security documentation and logs. This ensures they have access to necessary information, even if there are catastrophic provider incidents.
What is required to prove cloud compliance in a HIPAA audit?
When undergoing a HIPAA audit for a cloud environment, you must show that your cloud provider is compliant and that you have properly configured and managed your cloud resources. This means you need to keep records such as signed BAAs, compliance certifications from your cloud provider, records of your security configurations, policies for access control, and proof of regular security assessments. You should also have audit artifacts that are specific to the cloud, such as documentation for configuration management, settings for security groups, implementations of encryption, and logs of access from cloud environments. Many organizations use tools for continuous compliance monitoring that automatically produce much of this proof, which decreases the amount of manual work needed during audits and increases visibility of security on an ongoing basis.
Are there certain healthcare applications that should never be moved to the public cloud?
There are no hard and fast rules that prevent any type of healthcare application from being moved to public clouds, provided that the appropriate security measures are in place. However, some systems may pose a greater risk or be more difficult to implement, and these should be examined carefully. Legacy systems that use outdated security models, custom clinical applications that have hardcoded security assumptions, and systems that require specialized hardware integration can all pose significant migration challenges. The decision to move a system should be based on a thorough risk assessment that takes into account the specific application architecture, the sensitivity of the data being processed, compliance requirements, and the security measures that are available, rather than on general assumptions about the types of applications. For these more difficult applications, many organizations find that a hybrid approach works best, with the core components remaining in controlled environments and cloud capabilities being used where appropriate.
How do state-specific privacy laws affect decisions about moving to the cloud?
State privacy laws like the California Consumer Privacy Act (CCPA), New York SHIELD Act, and others create a complicated compliance environment that must be considered when designing cloud architectures. These laws often require more than HIPAA in terms of consent management, data subject access rights, and timelines for notifying about breaches. Cloud environments need to be designed with an understanding of where data is stored and the ability to implement compliance controls specific to each state based on the location of the patient. Organizations that operate in multiple states should either implement the most stringent requirements throughout their entire environment or develop sophisticated policy enforcement mechanisms that apply the appropriate controls based on jurisdiction. It is essential to work with legal counsel who have experience in healthcare privacy in the relevant states when designing cloud architectures that must comply with multiple regulatory frameworks.
When it comes to migrating to the cloud in healthcare, there’s a lot that needs to be considered. You have to plan meticulously, implement with expertise, and stay on top of compliance at all times. By understanding the ins and outs of different cloud models and putting the right security measures in place, healthcare providers can make sure they’re not only compliant with regulations, but also operating as efficiently as possible.
The cloud strategy you employ should be in line with the broader goals of your organization, offering the necessary security, compliance, and flexibility that contemporary healthcare provision requires. A careful, risk-based approach to adopting the cloud can help your organization to take advantage of the benefits of cloud computing, while also maintaining the trust of both patients and regulators.